Information on Diagnosing Silicosis
SILICOSIS
Essentials of Diagnosis
History of exposure to dust containing silicon dioxide (eg, hard rock mining, sandblasting, foundry work).
Characteristic x-ray changes: Bilateral nodules, fibrosis, hilar lymphadenopathy.
Recurrent respiratory infections.
Note: Tuberculosis is a common complication.
General Considerations
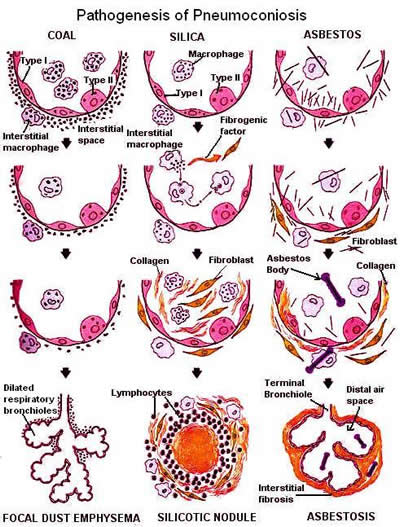
Silicosis is one of the chronic fibrotic pulmonary diseases caused by inhalation of inorganic occupational dusts .In the case of silicosis, free silica (silicon dioxide) is by far the most common offender. Prolonged exposure is usually required. Various immunoglobulins have been identified in silicotic tissue and in bronchoalveolar washings, but the exact role of immunologic factors in the pathogenesis of silicosis has yet to be demonstrated.
Clinical Findings
A. Symptoms and Signs: Symptoms may be absent or may consist only of unusual susceptibility to upper respiratory tract infections, "bronchitis," and pneumonia. Dyspnea on exertion is the most common complaint. It may progress slowly. Cough usually develops and is dry initially but later becomes produc tive, frequently with blood-streaked sputum. Severe, occasionally fatal hemoptysis may occur.
Physical findings may be absent in patients with advanced silicosis.
B. Laboratory Findings: Sputum studies for acid-fast bacilli are indicated to rule out silicotuber culosis or other mycobacterial infection. Pulmonary function tests characteristically show reduced lung volumes, decreased diffusion capacity, decreased compliance, and normal or increased flow rates. Lung biopsy is occasionally indicated to establish the diag nosis for compensation purposes.
C. X-Ray Findings: Chest x-rays are not diag nostic but often strongly suggest the diagnosis. Ab normalities are usually bilateral, symmetric, and pre dominant in the inner mid-lung fields. Small nodules tend to be of uniform size and density. Enlargement of hilar nodes is a relatively early finding. Peripheral calcification of the nodes, giving an "eggshell" appearance, may occur later. Interstitial fibrosis is man ifested by fine linear markings and reticulation. Coalescence of nodules produces larger densities, sometimes quite large (progressive massive fibrosis), which may have the radiologic appearance of a neo plasm. Associated emphysema gives an x-ray picture of increased radiolucency, often quite striking at the lung bases.
Silicosis Treatment
No specific treatment is available. Symptomatic treatment is indicated for chronic cough and wheezing. With TB associated Silicosis anti-tubercolosis drugs are adviced.
Lung Tissue with Crystalline SIlica Particles Embedded 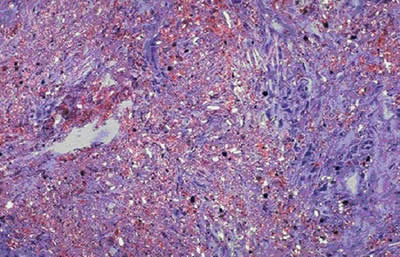 A typical silicotic lung nodule containing collagen fibres in a
whorled pattern 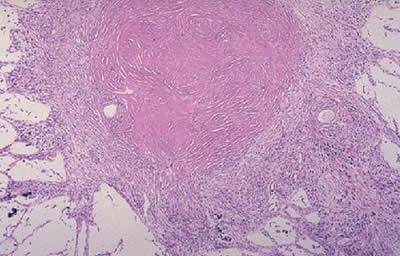
Tabulated Occupational Lung Diseases
| Disease and Occupation |
Causative Particle and Pathology |
Clinical Features |
X-Ray Findings |
Silicosis
(mining, drilling, blasting, grinding, abrasive menu- facture; venous other pro- cesses exposing silica to high temperatures, such as iron molding or ceramic manufacture) |
Free silica, cristobalite, and tridymite (toxic isomers produced by exposure of silica to high temperatures) cause rn- munologic tissue reactions producing nodules, fibrosis, lymphatic blockage, emphy sema, and hilar adenopathy. |
Required exposure is 2-20 years. May remain asymptomatic for years after lesions appear on x-ray. Then, dyspnea on exertion, dry cough, hemoptysis. Frequent infections, especially tuberculosis. Pulmonary insufficiency, chronic cor pulmonale. |
Nodules (inner, midlung fields), interstitial fibrosis, hilar adenopathy; peripheral ("eggshell") calcification of hilar nodes. Signs of associated tuberculosis )inflamma tory infiltrates, cavitation) may be present. |
Asbestosis
(asbestos mining and pro- ceasing, handling asbestos products) |
Iron, calcium, and magnesium silicates; chrysotile, amosite, crocidolite. Causes diffuse pulmonary fibrosis, thickened alveolar walls, pleural plaques, ferruginous (asbestosis) bodies in the tissue. |
Exposure is usually pro- longed but may be short, Lesions appear years after exposure. Increased incidence of bronchogenic carcinoma and malignant mesothelioma even after trivial exposure. |
Fine, diffuse infiltrates in lower lobes, with late appearance of interstitial fibrosis. Thickening and sometimes calcification of pleura, which may occur without parenchymal changes. |
Berylliosis
(beryllium production, machining, and drilling; use of beryllium alloys and ceramics in the electronics and space vehicle industries) |
Beryllium particles. Acute:Patchy infiltrations reaem- bling bronchial pneumonia. Chronic: Alveolar septal granuloma causing fine nodules. Fibrosis not prominent, Elastic tissue damaged, carcinoma emphysema. No hilar adenopathy. |
Acute: After a few weeks of exposure, upper respiratory symptoms; "bronchitis," "pneumonia" later. Chronic:Required exposure 6-18 months. Dyspnea, cough, weight loss, cyanosis, skin lesions, pulmonary insufficiency, cor pulmonale. |
Acute: Clear at first, then patchy infiltrations. Chronic: Scattered minute ("sandpaper") nodules. Later, larger nodules, diffuse retic ular markings. No hilar adenopathy. |
Bauxite pneumoconiosis
(Shaver's disease; aluminosis) |
May be due to other toxic contaminants rather than aluminum dust per Se, causing fibrosis, hilar adenopathy, atelectasis. |
Required exposure is several months to 2 years. Dyspnea (marked pulmonary insufficiency). Attacks of spontaneous pneumothorax |
Hilar and mediastinal adenopathy, irregularity of diaphragms, fibro sis, emphysema |
Anthracosis
(rarely dissociated from silicosis) (mining, city dwellers) |
Coal dust, causing black dis- coloration of lungs, nodes, distant organs (nodules rare). |
Progressive disease (fibrosis, emphysema) reported in Welsh soft-coal workers. Silica may be an important factor. |
"Reticulation," fine nodules. Coal dust may produce large densities by deposition without fibrosis. |
Siderosis
(iron ore processing, metal drilling, electric arc welding) |
Iron oxides, metallic iron, causing "red" (oxides) and "black" (metallic) discoloration of lung. "Red" type leads to fibrosis. "Black" type associated with silicosis. |
Findings are those of associated silicosis. (See above.) |
Dependent mainly on associated silicosis. |
|
|
|
|
Disclaimer: The liability of SMI ANALYTICAL is limited to the cost of analysis. SMI ANALYTICAL indemnifies
itself from any legal action which may be instituted against it due to supplied data. SMI ANALYTICAL accepts
no responsibility whatsoever for any results released, however used. No part of this document may reproduced
in part or in full unless permission from SMIANALYTICAL is granted in writing. This document may not be altered
in any way whatsoever and is printed without correction.
|
|